Dr Westermann is Deputy Director of the Department of General and Interventional Cardiology, University Heart Centre Hamburg. He is a specialist in Internal Medicine and Cardiology.
Dr Westermann opened his talk by reminding the audience of the surprising findings of the intraaortic balloon pump (IABP) SHOCK II study, which showed that the use of an IABP did not significantly reduce 30-day mortality in patients with cardiogenic shock (CS) complicating acute myocardial infarction.1 Alternative methods of treating CS have, therefore, been sought. Many doctors have turned to using extracorporeal membrane oxygenation (ECMO) to support these patients. Dr Westermann presented unpublished data from a large study (n=9,258) that showed a rapid growth in the use of ECMO in Germany from 2007–2014.2 Survival at 30 days was lower in patients over 65 years old and in those who required cardiopulmonary resuscitation (CPR). Using these data, an ECMO mortality score has been developed and validated.2 However, prolonged use of ECMO (>2 days) is associated with greatly increased mortality.3 The use of ECMO presents a number of clinical challenges. In particular, Dr Westermann highlighted that ECMO leads to an increased ventricular afterload. This increased afterload can become pathophysiological in ECMO patients causing vascular complications (bleeding, ischaemia, embolism), increased left ventricular (LV) filling pressures, increased in LV wall stress, pulmonary congestion, and the watershed phenomenon. The solution to this pathophysiological haemodynamic derangement is to vent the ECMO patient and relieve increased LV pressures and volume.
Recently, Dr Westermann’s team has investigated a different LV venting strategy in ECMO patients. The addition of VA-ECMO leads to decreased stroke volume and a right-shift of the pressure-volume loop. This increased afterload is due to retrograde femoral flow in CS. This causes further ECMO-dependent increases in LV wall stress and LV pressures, conditions that are unfavourable to the patient. Therefore, there is a need to shift pressure-volume loops to the left, which can be achieved by unloading the LV. This can be achieved through transseptal methods (e.g. atrioseptostomy, TandemHeart) or the less invasive transvalvular route (e.g. Impella). Dr Westermann suggested that the use of the Impella in addition to VA-ECMO may improve outcomes in patients with CS due to LV unloading.
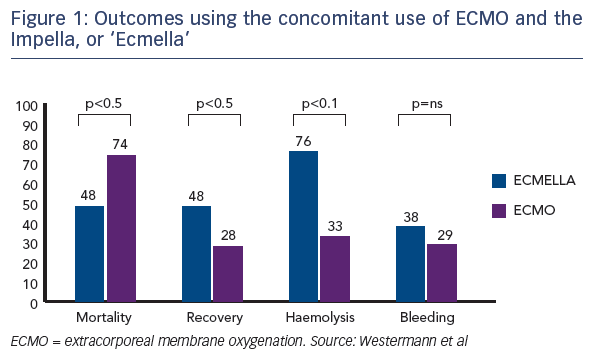
This hypothesis was tested in a study that enrolled 157 patients with CS: 123 received VA-ECMO support and 34 had concomitant treatment with VA-ECMO and an Impella device. A propensity-matching analysis was performed in a 2:1 ratio, comparing 42 patients undergoing VA-ECMO alone (control group) with 21 patients treated with VA-ECMO and Impella. Patients in the VA-ECMO plus Impella group (termed Ecmella) had a significantly lower rate of in-hospital mortality (47 % versus 80 %; P<0.001) and a higher rate of successful bridging to either recovery or further therapy (68 % versus 28 %; P<0.001) compared with patients receiving VA-ECMO alone.4 Similar findings have been observed in Dr Westermann’s recent registry study in Hamburg (n=81).5 There is increased haemolysis in the Ecmella group, but he indicated this did not lead to increased clinical complications. Those patients treated with ECMO/Ecmella also had significantly more rapid weaning from inotropes.
In conclusion, ECMO therapy may improve survival in CS; however, there is a lack of randomised controlled trial data. In addition, haemodynamic challenges remain with ECMO therapy in CS, including increases in afterload, LV wall stress, and pulmonary congestion. LV unloading with concomitant use of an Impella device may positively affect outcomes in patients with CS on VA-ECMO. It should be noted that data in support of this new concept have been derived from a registry study. Randomised controlled trial data are required. Nevertheless, Dr Westermann’s group have decided to use the Ecmella strategy as their clinical standard for future ECMO patients.
Concluding Remarks
In the closing remarks, Dr Kapur commented that the work presented has provided a huge breadth of research related to acute unloading and myocardial recovery, acknowledging the support of the sponsorship from Abiomed. Dr Anderson commented that this meeting represents an advance from last year and exciting and inspiring to see new thoughts and investigations that will further advance the field. He made special reference to Dr Fuster, whose passion for the cardiovascular field has driven him to accomplish so much. Dr Anderson hopes that passion for this new field of cardiology will encourage investigators to think outside the box. Dr Burkhoff concluded the meeting by acknowledging the quality of the presentations and posters, which is unprecedented in an emerging field. While he recognised the unique advantages of being a small group in a unique setting, he encouraged future growth of the A-CURE group.