The debate over the optimal mode of revascularisation for unprotected left main (ULM) coronary artery disease intensified with the advent of drug-eluting stents (DES). Professional society guidelines addressing ULM disease have been revised at an increasing frequency,1,2 the significance of randomised comparisons has been variously interpreted, and observational comparisons have become a veritable cottage industry. Making matters even more complicated, the debate is often depicted in simplified, polarised terms in the lay press and at national meetings. Not surprisingly, patients and clinicians alike are often left confused. The intention of this review is to place the ‘debate’ in context and highlight a few of the crucial issues in generalising the evidence base for those who manage ULM disease in clinical practice.
The Evolution of the ‘Gold Standard’
Coronary artery bypass graft (CABG) surgery had been unchallenged as the standard of care for patients with ULM disease for decades. Before addressing the evidence for percutaneous coronary intervention (PCI) as an alternative, it is important to briefly consider the quality of that supporting CABG as an alternative to medical therapy for ULM disease. Only two of the seminal randomised trials comparing CABG with medical therapy included patients with left main disease.3,4 A pooled analysis of these patients revealed a significant survival advantage for CABG with a relatively large treatment effect (odds ratio [OR] 0.32, 95 % confidence interval [CI] 0.15–0.70 p=0.004).5 Observational data gave support to this finding,6 and the paradigm of CABG to prolong longevity for left main disease remained essentially unchallenged for three decades.
There are important caveats concerning these early randomised trials that warrant emphasis. First, only 150 patients in total were randomised, quite a small number by contemporary standards. Second, they represent a pooled subgroup analysis and should be viewed with the attendant limitations of such analyses.7 Third, and perhaps most importantly, both surgery and medical therapy have evolved tremendously over the ensuing decades. CABG now routinely includes the use of mammary conduits, and surgical mortality has improved considerably – in the registry component of the Coronary Artery Surgery Study (CASS) it was over 4 % for patients with left main disease, a rate that most would consider unacceptable today. Conversely, ‘medical therapy’ at the time of these trials consisted of digitalis, beta-blockers and nitrates. Not even aspirin was routinely administered. Suffice it to say, the evidence base for the longevity benefits of CABG over medical therapy for treating left main coronary disease is neither large nor current.
Observational Trials of Coronary Artery Bypass Graft for Unprotected Left Main Disease
Although randomised clinical trials (RCTs) are considered the most robust assessment of efficacy, they have important limitations. Patients in RCTs tend to be younger, more often male and have fewer co-morbid conditions.8 Generalising results from these trials must therefore be done with caution. For example, the vast majority of patients in the aforementioned Veterans Affairs and European studies were under 60 years of age and most had stable symptoms. It is therefore tempting to use observational data from ‘real-world’ practice to supplement that from RCTs. However, accounting for bias in observational studies is challenging. As mentioned above, observational data have been used to support the value of CABG in prolonging life for patients with left main coronary artery (LMCA) disease. However, most observational trials include patients who have varying degrees of suitability for CABG. Poor surgical candidates are less likely to undergo surgery, and are also more likely to suffer adverse outcomes by virtue of the conditions that confer poor candidacy for surgery. The presence of a such a selection bias in observational comparisons of CABG and medical therapy was raised over three decades ago.9 Accounting for this bias remains even more imperative today if we are to leverage large and increasingly sophisticated observational registries and administrative data sets to make valid conclusions.
Challenging the Gold Standard – Drug-eluting Stents for Unprotected Left Main Disease
Initially, PCI for ULM disease was reserved for patients ineligible for CABG. With the emergence of DES, PCI has been more commonly used in patients who previously would have been treated with CABG.10 There have been over 4,000 patients included in observational comparisons of PCI with CABG for ULM disease.11–21 The duration of follow-up in these studies has ranged from one to five years. Meta-analyses including many of these trials have also been performed.22,23 A common finding of these studies has been comparable mortality following PCI or CABG, with patients undergoing PCI more likely to have repeat revascularisation procedures. However, these observational studies typically include patients with varying degrees of surgical eligibility, making treatment selection bias a potential limitation. This bias can confound these studies if the conditions responsible for poor surgical candidacy are independently associated with worse outcomes. To account for such potential ‘confounding by indication’, various statistical methods are commonly employed, including standard multivariable regression or Cox proportional hazards analyses, methods utilising inverse probability weighting (propensity scoring and matching) and instrumental variables. However, robust as these methods may seem, with the possible exception of instrumental variables (the least frequently used), they are ultimately dependent upon measured variables.24 If the conditions responsible for poor surgical candidacy are not measured, then confounding by indication compromises the validity of these observational comparisons.
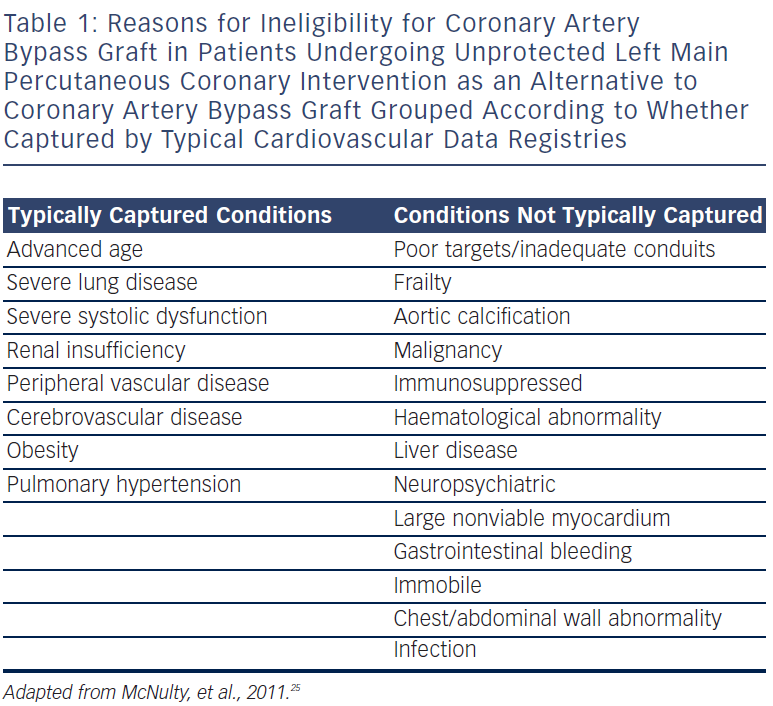
Most cardiovascular studies measure typical cardiovascular risk factors. However, the reasons PCI is selected instead of CABG for treating patients with ULM disease are often a consequence of clinical conditions not captured by typical cardiovascular data sets; despite a proliferation of observational comparative effectiveness studies, the reasons for surgical ineligibility have been poorly characterised. Using mixed methods, we found that the majority of patients undergoing ULM PCI as alternative to CABG at our institution had reasons for surgical ineligibility that were not typically measured by a standard cardiovascular data registry (see Table 1).25 If unmeasured, these conditions could still confound observational comparisons despite adjusting with the most commonly employed techniques to account for bias, including propensity scoring or matching. While unmeasured clinical conditions generally bias outcomes against PCI, patients with more complex anatomy are more likely to undergo CABG; since severity of disease is also associated with outcome, this could also lead to a selection bias. While observational comparisons can provide insight into real-world practice, their limitations need to be carefully considered.
Coronary Artery Bypass Graft Versus Percutaneous Coronary Interventions for Unprotected Left Main Disease – Randomised Trials
There have been three small randomised trials in the DES era comparing CABG with PCI for ULM disease and one large subgroup of a larger RCT. The first was the Study of Unprotected Left Main Stenting Versus Bypass Surgery (LE MANS) trial. One hundred and five patients with ULM disease were randomised to CABG or PCI, with 35 % of the patients in the PCI arm receiving DES. This study showed similar rates of one-year cardiac death, myocardial infarction (MI), stroke or repeat intervention.26 In a study of 201 patients, Boudriot et al. found that PCI with sirolimus-eluting stents (SES) was inferior to CABG for the combined endpoint of cardiac death, MI or repeat revascularisation.27 Most recently in the Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease (PRECOMBAT) trial of 600 patients with ULM disease, PCI with SES was non-inferior to CABG for the combined endpoint of death, MI and repeat revascularisation.28 However, the non-inferiority margin chosen was wide and the observed event rate in the CABG arm lower than expected. This led to a somewhat liberal interpretation of ‘non-inferior’ whereby a doubling of event rates in the PCI arm would still be considered non-inferior. Finally, in the subgroup of 705 patients with ULM disease in the TAXUS Drug-Eluting Stent Versus Coronary Artery Bypass Surgery for the Treatment of Narrowed Arteries (SYNTAX) trial, patients undergoing PCI with paclitaxel-eluting stents had similar combined three-year rates of death, MI, stroke or repeat revascularisation to those undergoing CABG. PCI was associated with a significant reduction in stroke (1.2 versus 4.0 %, p=0.02) but an increase in repeat revascularisations (20.0 versus 11.7 %, p=0.004) with no difference in all-cause death (7.3 versus 8.4 %, p=0.64).29 Although a ‘pre-specified subgroup’ of the SYNTAX trial, since the parent trial did not meet the goal of non-inferiority, these findings should be viewed as hypothesis generating. Recently, Capodanno et al. performed a meta-analysis incorporating the results of these three trials and the SYNTAX ULM subgroup.30 At one-year there was equivalence in terms of death with fewer strokes and more repeat revascularisation procedures in patients undergoing PCI. Although there have been an order of magnitude, more patients randomised between DES versus CABG for the treatment of ULM disease than for CABG versus medical therapy, the duration of follow-up has been limited; the possibility of a late difference in mortality or MI cannot be excluded.
While the clinical endpoints discussed above are often combined to obtain adequate power for clinical trials, the concept of ‘major adverse cardiac and cerebrovascular events’ (MACCE) is not always easy to convey to patients. Even among clinicians, there have been debates as to whether excess repeat revascularisation procedures are ‘offset’ by fewer strokes, and as to whether a MI should be weighed as heavily as a death.31 Although it is tempting to address potential adverse outcomes individually for each mode of revascularisation, the limited nature of the data, especially in terms of the duration of follow-up, makes such post hoc ‘parsing’ challenging, and translating this information to facilitate true shared decision-making is problematic.
Endpoints – Major Adverse Cardiac and Cerebrovascular Events or Quality of Life?
Many have argued that even broad composite endpoints such as death, MI, stroke or repeat revascularisation are inadequate to compare true morbidity, and that additional outcomes taking into account post-procedure recovery ought to be measured for a more accurate comparison of CABG and PCI. Fortunately, well-validated instruments measuring health status have been applied in this regard, most recently in the SYNTAX trial. Early after revascularisation, overall quality of life was much worse with CABG than for PCI (on the order of having symptomatic heart failure or lung disease). However, by one-year this difference had disappeared with CABG being associated with a significant but not clinically meaningful improvement in angina frequency and no difference in overall quality of life.32 For the left main subgroup, there was no difference in angina frequency at one-year. Whether short-term quality of life benefits are important is a subjective question that will vary depending on individual patient and family circumstances. For someone self-employed in a difficult economic position, the prospect of a short recovery might outweigh the potential for repeat procedures, whereas for someone with sufficient social supports, CABG offers the time-tested opportunity to reduce future trips to the hospital at the expense of a few difficult months. Of course, short-term quality of life gains must be carefully weighed against long-term survival benefits in subpopulations where CABG is the superior therapy.
Selective Use of Percutaneous Coronary Intervention – Anatomic Stratification?
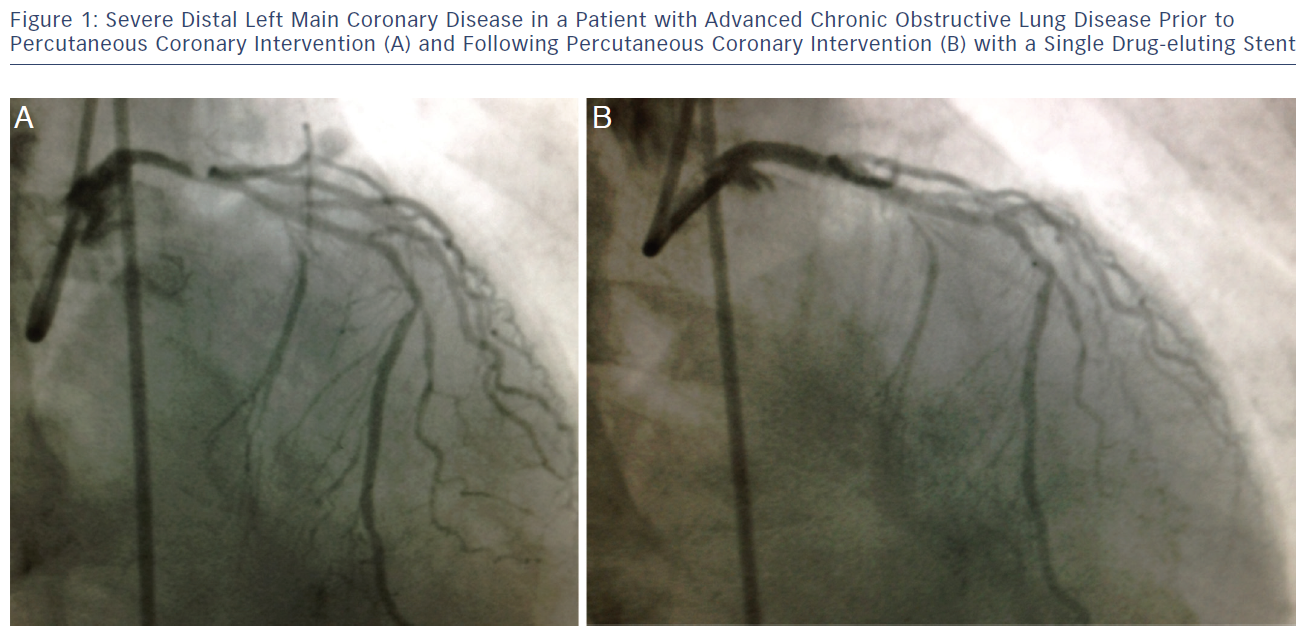
Up to this point we have treated ULM disease uniformly in comparing treatments. Obviously there are clinical and anatomic differences in patients with ULM disease, and these will have a bearing on outcomes following PCI or CABG. Professional society guidelines now advocate using indices of the anatomic complexity disease such as the SYNTAX Score33 to aide in the triage of patients with ULM disease to PCI or CABG.1,2 This is supported by evidence from the SYNTAX trial, where three-year rates of MACCE (death, stroke, MI and repeat revascularisation) were higher in patients with intermediate and high SYNTAX scores (indicating more complex anatomy).29 In the subgroup of patients with ULM disease, MACCE was similar for patients with low (0–22) or intermediate (23–32) SYNTAX scores, but far worse for those with high scores treated with PCI. Approximately one-third of patients screened for the SYNTAX trial were excluded for having anatomy that precluded PCI. If one also considers these patients, then the majority of those with ULM disease had SYNTAX scores >33. An anatomic consideration that deserves special attention is involvement of the distal left main bifurcation (see Figure 1). Observational data has demonstrated worse outcomes for patients undergoing PCI for distal ULM disease,34,35 and patients with higher SYNTAX scores are more likely to have distal bifurcation involvement.
While it is tempting to conclude that patients with less complex anatomy, especially without distal bifurcation involvement, fare equally well after PCI or CABG, it is important to remember that this conclusion is based on inferences from analysing a subgroup (lower SYNTAX scores) of a large subgroup (those with left main disease) within a trial in which non-inferiority was not demonstrated for the parent study population. In that light it is interesting that professional societies should endorse such an approach when these results have been described as ‘hypothesis generating’ by the study authors. At the present time, given worse outcomes associated with PCI for distal left main disease, for patients who are reasonable surgical candidates with severe disease extending into both the adjacent circumflex and left anterior descending arteries, current evidence favours CABG as the optimal mode of revascularisation.
Selective Use of Percutaneous Coronary Intervention for Unprotected Left Main Disease – Stratification by Surgical Risk?
PCI has long been an option for ULM disease in patients with ‘prohibitive surgical risk’. However, prohibitive surgical risk has been poorly characterised. While risk scores developed for cardiothoracic surgery have been shown to predict outcomes following PCI for unprotected left main coronary artery (ULMCA),36 these risk scores measure typical cardiovascular risk factors; as discussed earlier, the conditions rendering patients ineligible for CABG are often not typical risk factors. Risk scores can never replace clinical judgment, and patients with similar scores can vary markedly in terms of surgical candidacy. It is also likely that in some patients even PCI as an alternative to medical therapy is not likely to offer meaningful benefit and may in fact cause harm; the utility PCI, especially in the ‘frail phenotype’, should be the focus of further investigation.
Medical Therapy for Unprotected Left Main Disease?
Often overlooked in the heated rhetoric regarding the optimal mode of revascularisation for ULM disease is the basic issue of what constitutes significant left main disease in the first place, and whether in fact medical therapy alone might be sufficient treatment for some patients. Although a diameter stenosis of >50 % is typically considered ‘significant’, there is substantial interobserver variation in the angiographic assessment of left main disease and poor correlation of visual assessment with haemodynamically significant disease.37,38 Largely forgotten is the finding that the mortality advantage of CABG over medical therapy among patients with ULM disease in the CASS Registry was confined to patients with reduced systolic function and diameter stenoses >70 %.6,39 With the evolution of medical therapy, recent investigations have assessed the role of medical therapy alone for ‘intermediate’ or ambiguous LMCA. Both intravascular ultrasound40 and fractional flow reserve (FFR) guided38 approaches have shown equivalent outcomes if PCI is deferred in patients with minimum lumen area >6 mm2 or FFR >0.80. The role of medical therapy alone, especially in minimally symptomatic patients with normal systolic function or for more moderate incidentally discovered disease, should not be discounted.
Putting it Together – The Present
Now that professional society guidelines have endorsed PCI as an option for the treatment of ULM disease in a subset of patients eligible for CABG, how are we to best incorporate this into present clinical practice? Guidelines also advocate a ‘heart team’ approach in which patients receive counselling on the merits and risks of PCI and CABG from a team of individuals consisting of at least one cardiologist and one cardiothoracic surgeon.41 While this certainly sounds like good medicine, implementation in practice is likely to be challenging. Cardiologists typically dictate decisions regarding the mode of revascularisation, and for patients with ‘surgical disease’ the recommendation regarding the mode of revascularisation most often comes from the catheterisation laboratory cardiologist.42 Soliciting a ‘surgical opinion’ is a laudable goal, but which surgical opinion? A colleague in a multispecialty practice? One less inclined to operate? If there are revenue implications, should the patient be informed? Conversely, for patients at high risk of complications with CABG in whom ad hoc ULM PCI is feasible, should the patient be taken off the table and subjected to the risks and inconveniences of a separate procedure simply to satisfy a ‘formality’? Finally, as any clinician who has encountered this situation can attest, some patients are likely to be overwhelmed with the information and true ‘shared decision-making’ will be difficult if not impossible. Research into decision aides for both patients and clinicians and other models is desperately needed to clarify the most effective strategy for facilitating informed and transparent decisions.
Future Directions
Finally, this debate will likely forever be over a ‘moving target’. As we digest evidence from trials and incorporate them into practice guidelines, devices, techniques and medical therapies evolve in the interim such that the older data become potentially obsolete and less relevant to contemporary practice. For example, while the SYNTAX trial is a useful source of data, some have suggested the results would have been more favourable for PCI with ‘second-generation’ DES.43 Second-generation DES are being compared with CABG in the ongoing Evaluation of XIENCE PRIME™ Everolimus Eluting Coronary Stent System (EECSS) or XIENCE V® EECSS Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL) and Nordic-Baltic-British Left Main Revascularization Study (NOBLE) trials, both large, well-powered trials.
Conclusions
Medical, percutaneous and surgical therapy for ULM disease has improved dramatically over the past three decades. Along with these improvements, decisions regarding the optimal mode of revascularisation have become more complicated with both PCI and medical therapy being viable options in a subset of patients. Identifying the subset appropriate for alternatives to CABG and translating the risks and benefits of these alternatives to individual patients in a transparent fashion is no simple matter. While clinical and anatomic scores may be helpful in this regard, they are no replacement for clinical judgment and the ‘art’ of medicine.