Dr Meraj is an Interventional Cardiology Specialist at the Hofstra Northwell Health School of Medicine in New York.
Dr Meraj began his presentation with an overview on the current treatment paradigm in acute myocardial infarction (MI) with or without cardiogenic shock (CS), which focuses on primary perfusion in the first 2 hours. In acute coronary occlusion, time is of the essence, and the relationship between shorter door-to-balloon (DTB) times and improved outcomes is well established. Maximal benefit of reperfusion therapy is observed when the therapy is applied within 2 hours of the patient presenting at the hospital.1 This has led to the adoption of a target 90 minutes DTB time. However, the maximal effect of DTB time may have been reached. Recent data have indicated that while the average DTB has fallen well below 90 minutes, a corresponding drop in mortality rates of MI patients has not been observed.2 Additional strategies are therefore needed to reduce in-hospital mortality rates in this population.
Understanding the balance between myocardial oxygen supply and demand in MI has enabled us to develop effective left ventricle (LV) unloading protocols.3,4 Numerous preclinical investigations have supported the hypothesis that primary LV unloading and delaying coronary reperfusion provides both cardioprotective signalling and myocardial salvage. These scientific investigations have in part led to a recent paradigm shift in acute MI management that proposes door-tosupport time as an emerging target of therapy to reduce reperfusion injury and improve outcomes associated with MI/CS.5
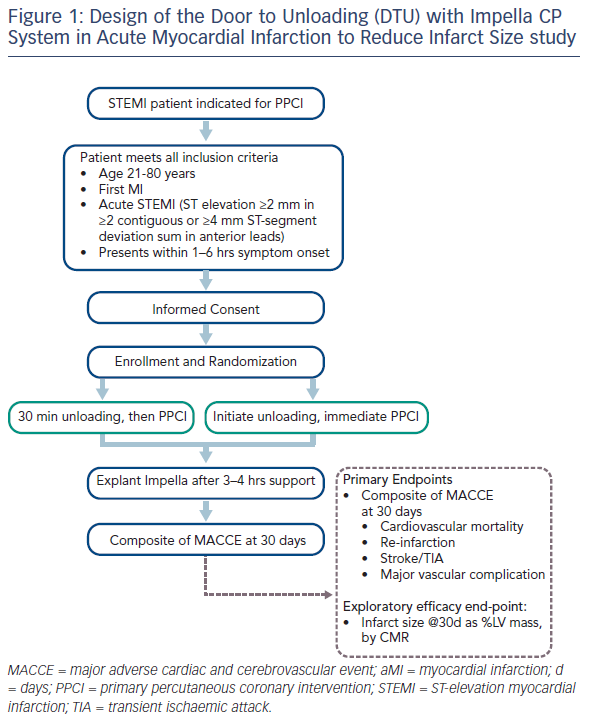
In late 2016 the US Food and Drug Administration gave approval for the Door to Unloading (DTU) in ST-segment elevation MI (STEMI) safety and feasibility study. This study is a prospective feasibility study to evaluate the use of the Impella CP device for unloading of the LV prior to primary percutaneous coronary intervention (PPCI) in patients presenting with acute STEMI, without CS.6 The main inclusion criteria are age 21–80 years, first MI and acute anterior STEMI with ≥2 mm in two or more contiguous anterior leads or ≥4 mm total ST-segment deviation sum in the anterior leads, and presentation between 1 and 6 hours of symptom onset.
Patients are randomised to two treatment arms: immediate Impella implantation followed by 30 minutes of mechanical unloading prior to PPCI, or immediate Impella implantation directly followed by PPCI. The Impella is explanted after 3–4 hours of support. This time was chosen as the optimal unloading time is not known and the implications for leaving in a 14 Fr sheath for longer than 4 hours may have safety implications. The primary endpoints are the composite of cardiovascular mortality, re-infarction, stroke or transient ischaemic attack, major vascular complication at 30 days, and also an additional exploratory efficacy endpoint of the infarct size as percentage of LV mass, evaluated by cardiac magnetic resonance (CMR) at 30 days post- PPCI (see Figure 1).
The first patient was enrolled in April 2017. To date, all patients have met the <90 min DTB times, including those who had delayed reperfusion. The DTU metric will be determined for each patient as the study continues. We will need an understanding of 3- to 5-day and 30-day magnetic resonance imaging (MRI) to guide optimisation of infarct size reduction. Results from these patients will be used to guide best practices for the pivotal study. Given the design of the study and its time-sensitive nature, enrolment decisions are based only on the patient history taken at the time of initial presentation. It can be difficult to explain the treatment and precisely ascertain clinical symptom start time. A radial approach is used for access for the non-large bore site to reduce unnecessary vascular complications. Patient screening should also be considered to enable adequate MRI; some patients may be claustrophobic and unable to undergo the procedure, an unanticipated complication of the study design. Other clinical considerations include the completeness of revascularisation in STEMI, use of adjunctive pharmacotherapy during Impella support, duration of Impella support after PPCI, and access site management, i.e. removal of the pump using manual compression or pre-close suture.
In summary, this ongoing study has a strong focus on safety, using large bore access and device therapy. Appropriate patient selection is key to help us to understand the physiology and clinical correlates to DTU and how to use concomitant therapies to improve patient outcomes.








