The coronary tree is comprised of arteries which divide into ever smaller branches to supply the myocardium. This means that the diameter of the vessel proximal to a bifurcation is always larger than the diameter of the main vessel distal to the bifurcation. The proximal optimisation technique (POT) was proposed by Dr Olivier Darremont as a technique to compensate for this difference in diameters when bifurcation lesions are stented. The technique is fully supported by the European Bifurcation Club and is a key part of the consensus statement produced by this group of experts.1 A short balloon is expanded in the proximal main vessel just up to the carina. This enables full expansion and complete apposition of the stent in the proximal main vessel. In addition, the POT also facilitates re-crossing into the side branch in order to optimise the final result if required. The following review article describes how to perform the technique and presents the evidence to support its routine use.
Murray’s Law
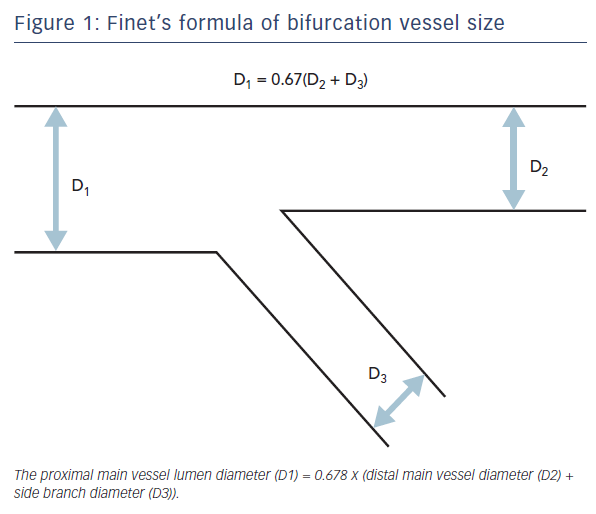
The coronary tree is composed of vessels which branch into vessels of decreasing diameters. This follows Murray’s Law which states that the radii of daughter branches are related to the radius of the parent branch. Therefore, at each branch point within the coronary tree, the diameter of the vessels can be predicted. Professor Gérard Finet simplified Murray’s Law and showed that the proximal main vessel diameter closely approximates to the sum of the daughter vessel diameters (distal main plus side) multiplied by 0.67 (Figure 1).
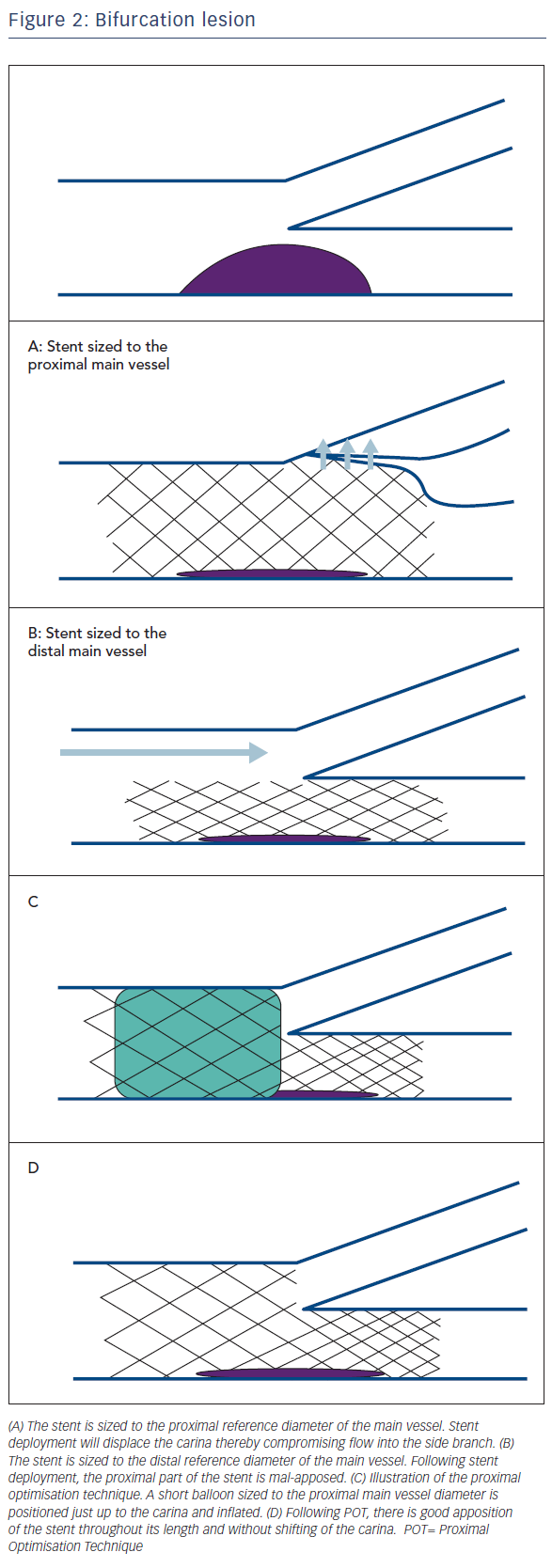
Therefore, for all bifurcations, the diameter of the distal main vessel will be consistently smaller than the diameter of the proximal main vessel. The greater the diameter of the side branch, the greater is the disparity between the diameter of the proximal main vessel and the vessel distal to the bifurcation. This difference in diameters is important when selecting a stent of appropriate diameter. If a stent is chosen based on the diameter of the proximal main vessel, this will be ‘over-sized’ for the distal main vessel. This may be associated with compromise of flow into the side branch as it can lead to shifting of the carina (Figure 2A). However, if the stent is chosen based on the diameter of the distal main vessel, the proximal part of the stent will be small relative to the vessel size (Figure 2B). This mal-apposition has implications particularly if a new guidewire is advanced through the stent as it may inadvertently pass behind the stent struts. Any further balloon dilatation will then crush the stent potentially leading to major complications including stent thrombosis.2 Importantly, this may not necessarily be evident to the operator on angiography or by ‘tactile feedback’ of the smoothness of wire passage.
Technique
The aim of the POT is to fully appose the stent proximal to the bifurcation; in addition, POT expands the stent cells overlying the side branch ostium. A short balloon is taken and must be accurately positioned with the distal marker of the balloon placed at the carina, level with the side branch ostium (Figure 2C). This is best done by confirming a good position on orthogonal views. If positioned too distal, this could cause carinal shift, if too proximal then this will not appropriately expand the stent overlying the side branch ostium. If required, an additional balloon inflation is made more proximally to ensure that the inflow of the stent is fully apposed. To help accurately position the balloon, it is useful to use radiographic optimisation with techniques such as stent boost imaging. It is important to choose a correctly-sized balloon (non-compliant or semi-compliant) that will adequately expand the proximal part of the stent.
Evidence in Favour of POT from Bench Models
Bench models have been key to developing the concept of the POT and demonstrate the associated excellent anatomical / scaffolding result.3–6 In 2011, Foin et al.3 evaluated the concept in a bench model of commercially available stents. They demonstrated that a final POT was able to significantly improve the anatomical result following single stent implantation for a bifurcation, confirming the reduction in mal-apposition of the stent in the proximal main vessel. Furthermore, they also showed the potential downside of final kissing balloon dilation (KBD) which has traditionally been recommended in clinical practice. KBD caused asymmetrical stent (over)expansion in the region where both balloons were expanded together, as well as development of mal-apposition of the proximal part of the main vessel stent (Figure 3).
Computational simulations have been useful in assessing the negative impact of KBD. Studies have shown that in addition to creating elliptical deformation of the stent in the proximal main vessel, KBD also causes altered strut configuration, damage to the stent coating, as well as arterial injury to the side branch ostium.7–9 KBD results in higher stresses in the arterial wall10 and stent ‘over-stretch’ has been shown to increase the inflammatory response to stent implantation. Otake et al. demonstrated, by Optical Coherence Tomography (OCT), that stent asymmetry was correlated with stent thrombosis and an increased rate of major adverse clinical events (MACE) in patients treated with drug-eluting stents.11
Foin and colleagues went on to carry out a further bench study and proposed a step-wise post-dilation strategy in preference to KBD.4 In this second study, following stent implantation, they performed POT followed by side branch balloon-inflation. The final step was either KBD or a final POT. As before, KBD was shown to have unfavourable features causing elliptical over-expansion of the stent proximal to the carina, as well as distortion of the proximal part of the main vessel stent with development of mal-apposition (even though POT had been done prior to the KBD). However, the step-wise approach (POT, side branch dilation, then re-POT) led to a more favourable result with significantly less strut mal-apposition at the proximal edge of the stent. In addition, POT expanded the stent cell overlying the side branch ostium. This is advantageous as it has the potential to make it easier to re-cross a guidewire into the side branch and may also facilitate ‘optimal re-cross’. When a provisional strategy is used, re-cross should ideally be performed through a distal stent cell.12 This ensures that balloon inflation will produce better clearance of struts from the side branch ostium.
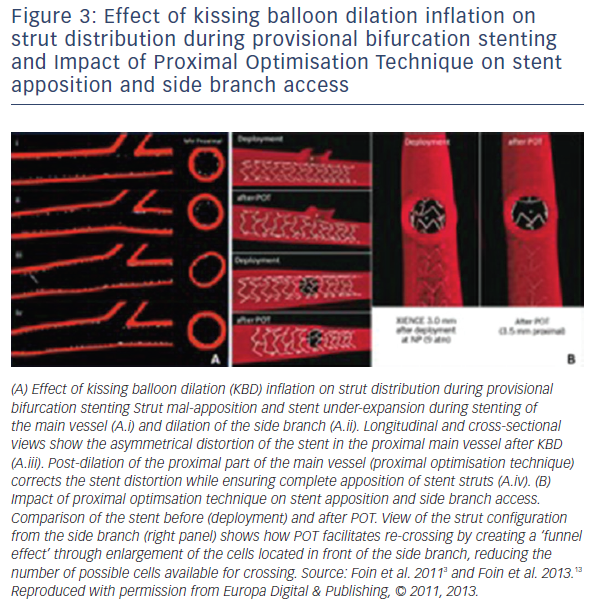
The studies by Foin have been subsequently supported by a further bench model study6 that evaluated six strategies: (i) KBD alone, (ii) POT then KBD, (iii) POT then asymmetrical KBD with the main vessel balloon inflated and maintained at 12 atm and the side branch balloon inflation reduced from 12 atm to 4 atm, (iv) POT then asymmetrical KBD with side branch balloon inflated and maintained at 12 atm and the main vessel balloon inflation reduced from 12 atm to 4 atm, (v) POT then side branch inflation (SBI), (vi) POT then SBI at 12 atm then re-POT.6 Each strategy was evaluated in two different stent designs. The results demonstrated that the best geometric result was obtained from POT – SBI –re-POT. Compared to techniques utilising KBD, the POT – SBI – re-POT strategy reduced the proximal area overstretch and restored circularity, reduced the side branch ostium stent-strut obstruction, and significantly reduced global strut mal-apposition (from 40 ± 6.2 % to 2.6 ± 1.4 %).
This reduction in strut mal-apposition may have important clinical implications as strut mal-apposition disturbs blood flow causing high shear stress. This activates platelets and has been shown to delay neointimal coverage of struts, both potentially increasing thrombogenicity and the potential for late stent thrombosis.14,15 Furthermore, disturbed flow patterns caused by the geometrical complexity of bifurcation lesions may explain the relative increase in the risk of developing restenosis.16
Recently, Murasato et al.5 used a bench model to suggest that a compliant balloon may be preferable to the use of a non-compliant balloon to optimise strut apposition during POT. High pressure is not a pre-requisite as the balloon merely needs to dilate the unopposed stent; however, an adequately large balloon diameter is obligatory. For some larger vessels, the expansion range of non-compliant balloons will limit their ability to fully appose the struts whereas the greater expansion range of a semi-compliant balloon could be advantageous. For example, if a vessel is 4.9 mm diameter, a 4.5 mm non-compliant balloon may only reach a maximal diameter of 4.8 mm whereas a semi-compliant balloon will easily expand to 5.0 mm.
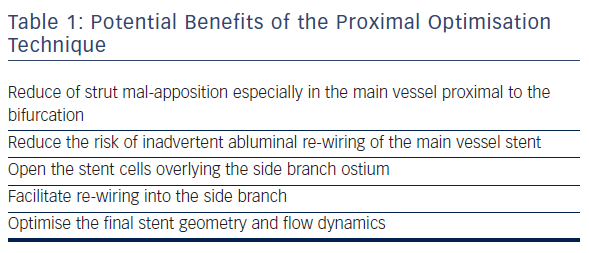
All of these bench studies provide evidence to support the potential benefits of POT (Table 1) and emphasise the importance of always completing the procedure with a final POT. This can correct both the mal-apposition as well as improve the elliptical shape back to a circular lumen which will favourably influence the flow dynamics. This information forms the basis by which experts including the European Bifurcation Club have adopted and strongly support the routine use of POT.
Implications for single stent bifurcation strategy
It is important to appreciate that the clinical trials evaluating various bifurcation strategies (e.g. one stent versus two-stent strategies) were performed prior to the widespread adoption of POT. However, there seems no reason why the important information obtained from bench model studies should not be incorporated into clinical practice.
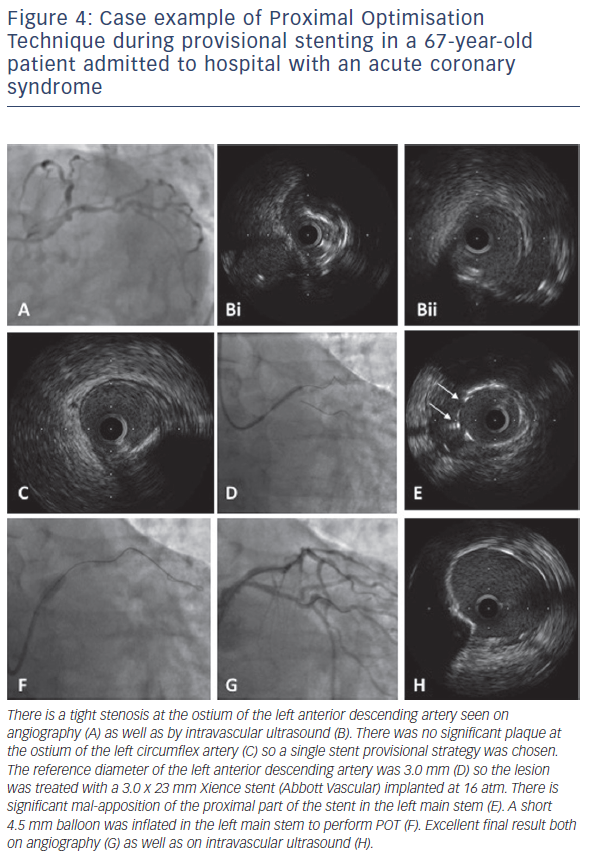
Randomised controlled studies have demonstrated that, for the majority of bifurcations, a single stent strategy is preferred over a twostent strategy; with recent data suggesting improved 5-year survival for the simpler technique.17 The recommendation from the EBC is that both vessels are wired, with pre-dilation of the main vessel if required.1 Pre-dilatation of the side branch is to be avoided if possible as, if this causes dissection, the side branch will be more difficult to re-wire once the main vessel has been stented. The main vessel is stented using a stent diameter based on the reference diameter of the main vessel distal to the bifurcation (Figure 4). The stent must be long enough to cover sufficient length of the proximal main vessel to allow POT to be performed, bearing in mind that the shortest available balloon may be 6 mm or 8 mm in length. After stenting, POT is performed to optimise stent expansion. In addition, this balloon dilatation will also open the stent cells overlying the side branch ostium and may partially scaffold the side branch ostium. In the majority of situations, the procedure can be terminated at this point. However, if there is concern regarding flow into the side branch, POT facilitates successful re-wiring of the side branch to enable further balloon dilatation +/- stent implantation. Based on information from the bench models, the procedure should always end with a final POT.
Although there is a lack of robust clinical data to demonstrate the advantages of POT, there is evidence from a randomised study to show that that there is no benefit (or perhaps a disadvantage) to undertaking KBD routinely.18,19 The NORDIC III trial randomised 477 patients with bifurcation lesions to final KBD versus no KBD after main vessel stenting.19 At 6 months, there was no significant difference in the primary endpoint of cardiac death, non-procedural myocardial infarction, target lesion revascularisation (TLR) or stent thrombosis (2.1 % versus 2.5 %, p=1.0). However, the KBD procedures were longer and utilised higher contrast use. The 5-year clinical outcomes of this trial were presented in 2015.20 There were no differences in the rates of myocardial infarction, TLR or stent thrombosis. Interestingly however, cardiac mortality was significantly higher in the group treated with routine KBD (4.2 % versus 0.8 %, p=0.02). Though this may be a chance finding, it could also be hypothesized that in the absence of routine POT, some of the late events might be due to inadvertent abluminal wiring occurring in the pursuit of performing KBD.2
The efficacy of KBD from registry data is contradictory. The first COBIS registry21 evaluated 1,065 patients of which 736 (69 %) were treated with KBD. At 22 months’ follow-up, there was a significantly higher rate of MACE in those treated with KBD (10.0 % versus 4.9 %, p<0.05), driven by a higher rate of TLR in the KBD group (9.1 % versus 3.4 %, p<0.05). The subsequent COBIS II registry demonstrated quite the opposite and suggested that KBD might in fact be favourable.22 This study evaluated 1,901 patients with a bifurcation lesion treated by single drug-eluting stent implantation. KBD was performed at the discretion of the operator in 620 patients (32.6 %), notably a lower proportion than that seen in the first COBIS registry. At a median follow-up of 36 months, those treated with KBD had a significantly lower rate of MACE (adjusted hazard ratio [HR]: 0.68, 95 % CI: 0.46 to 0.99; p=0.048). This benefit remained apparent after propensity score matching (545 pairs, adjusted HR: 0.50, 95 % CI: 0.30 to 0.85; p=0.01); with a significantly lower rate of TLR in the KBD group.
Ongoing in vivo work is being undertaken to evaluate POT in clinical practice and will potentially provide clinical evidence to back-up the evidence from bench studies. Studies have been designed that incorporate OCT imaging as a tool to identify stent strut malapposition, which is proposed as a surrogate marker for a higher risk of adverse clinical events.
Implications for a 2-stent strategy
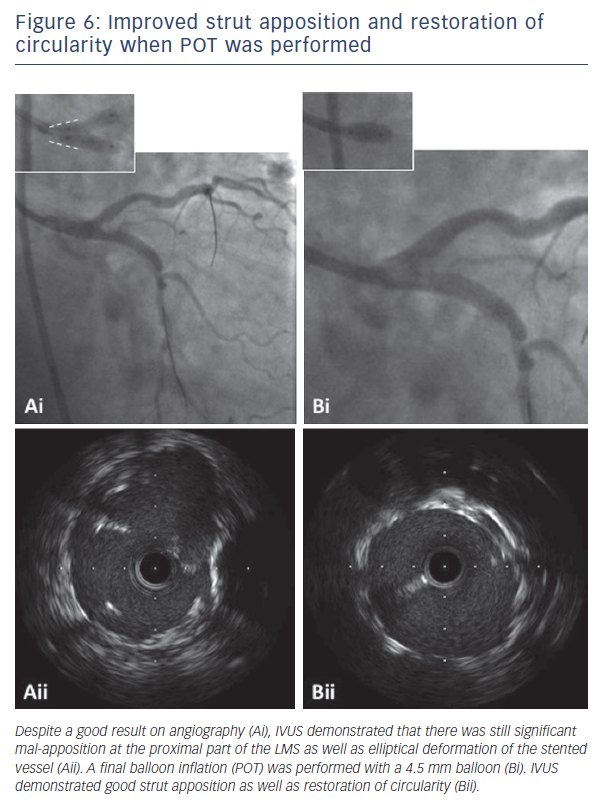
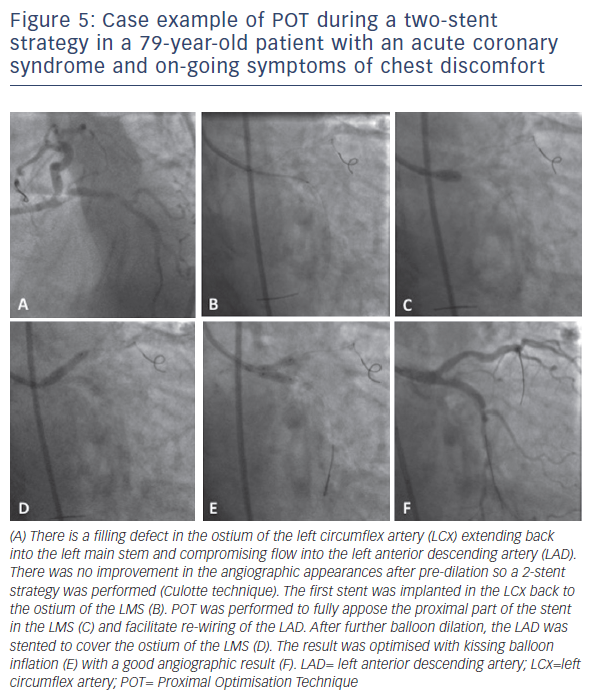
Whatever stenting technique is used, POT is an integral part of twostent strategies to appose the stent in the proximal main vessel as well as to open up the stent cells to facilitate easier guidewire crossing through the side of the stent. In contrast to a single stent strategy, there is strong evidence in favour of kissing balloon dilation for two-stent strategies.23,24 Failure to perform successful KBD is associated with both a greater rate of stent thrombosis as well as a significantly higher rate of restenosis, TLR and MACE. Indeed, some of the best clinical results have been obtained from the double kissing strategy of the DK-crush technique.25–27Figure 5 illustrates the principle of incorporating POT during two-stent bifurcation procedures. The first POT is performed after the first stent has been implanted, to appose the stent in the proximal main vessel and open the struts to facilitate optimal guidewire re-crossing. The second stent is implanted according to the preferred strategy, with further POT used as required to facilitate guidewire re-crossing. Final KBD is mandated, however, as demonstrated in Figures 5A and 6B, such KBD causes elliptical deformation of the stented proximal main vessel. This has the potential to impact negatively on the flow dynamics, but can be improved following a final POT which restores the circular morphology.28
The importance of POT to facilitate optimal guidewire re-crossing during two-stent bifurcation procedures is illustrated by a case report published by Wurtz and colleagues.2 They reported a patient who presented with stent thrombosis six years after undergoing Culotte bifurcation stenting. They showed, by OCT, that there had been inadvertent abluminal wiring during the original procedure. Instead of seeing a circular double layer of stent struts in the proximal main vessel, there was evidence that the side branch stent had been completely crushed in the proximal main vessel. This was not evident on angiography at the time of the index procedure. Importantly, this could have been avoidable if POT had been performed prior to re-wiring; however, this technique was not part of clinical practice at the time the original procedure was undertaken.
Bioresorbable scaffolds
Bioresorbable scaffolds (BRS) have some expansion limitations beyond which there is a risk of strut fracture.29 Therefore, when selecting the most appropriate size, it is important to appreciate the dilation limitations. The expansion capacity of the Absorb scaffold (Abbott Vascular, Santa Clara, California) allows post-dilation up to 0.5 mm above the nominal diameter. An ‘aggressive’ POT should be avoided for BRS so it may be necessary to choose a diameter that is a little larger than the distal main vessel reference diameter and closer to the proximal main vessel reference diameter. The scaffold is deployed at nominal pressure, and then optimised using both an appropriately-sized balloon for the distal part of the stent as well as a larger balloon for the POT. If the SB appears compromised, the recommended technique is POT, followed by balloon inflation in the side branch, followed by re-POT.30 Bench studies suggest that for a 3.0 mm Absorb scaffold implanted in the main vessel, the side branch can be dilated with (up to) a 3.0 mm balloon inflated to a maximum of 10 atm.31 Importantly, because of the risk of scaffold fracture with overstretch, KBD with overlapping balloons is strongly discouraged.1
Conclusion
The proximal optimisation technique is a key part of treating large bifurcation lesions and will optimise results of both single and twostent strategies. Technique is important – an appropriately sized balloon should be positioned and inflated just up to the carina. When performed well, the enhanced lesion scaffolding, reduced strut malapposition and improved flow dynamics are likely to translate into improved clinical results.